introduction
Scar is defined as ‘‘the fibrous tissue that replaces normal
tissue destroyed by injury or disease’’.(1) Causes of acne scar
formation can be broadly categorized as either the result
of increased tissue formation or, more commonly, loss or
damage of local tissue.(2)
Clinical manifestations of acne scars as well as severity of
scarring are generally related to the degree of inflammatory
reaction, to tissue damage, and to time lapsed since the onset
of tissue inflammation.(3, 4) There have been attempts to
classify acne scars in order to standardize severity assessments
and treatment modalities.(3, 4) However, consensus
concerning acne scar nomenclature and classification is still
lacking.(3)
clinical classifications
In 1987 Ellis et al. proposed an acne scar classification system
and utilized the descriptive terms ice pick, crater, undulation,
tunnel, shallow-type, and hypertrophic scars.(5) Langdon, in
1999, distinguished three types of acne scars: Type 1, shallow
scars that are small in diameter; Type 2, ice pick scars; and Type
3, distensible scars.(6) Lately, Goodman et al. proposed that
atrophic acne scars may be divided into superficial macular,
deeper dermal, perifollicular scarring, and fat atrophy based on
pathophysiologic features.(7)
One classification system frequently used in clinical practice
for acne scars is based on both clinical and histological
features.(8) Acne scars are classified into three basic types
depending on width, depth, and 3-dimensional architecture:
Icepick scar•• s: narrow (diameter < 2 mm), deep, sharply
marginated and depressed tracks that extend vertically to
the deep dermis or subcutaneous tissue.
•• Boxcar scars: round to oval depressions with sharply
demarcated vertical edges. They are wider at the surface
than icepick scars and do not taper to a point at
the base. These scars may be shallow (0.1–0.5 mm) or
deep (≥ 0.5 mm) and the diameter may vary from 1.5
to 4.0 mm.
•• Rolling scars: occur from dermal tethering of otherwise
relatively normal-appearing skin and are usually
wider than 4 to 5 mm in diameter. An abnormal fibrous
anchoring of the dermis to the subcutis leads to superficial
shadowing and to a rolling or undulating appearance
of the overlying skin.
Other clinical entities included in this classification are hypertrophic
scars, keloidal scars, and sinus tracts.(8) Both hypertrophic
and keloidal scars result from an abnormal excessive tissue
repair: clinically, hypertrophic scars are raised within the limits
of primary excision, whereas keloidal scars transgress this
boundary and may show prolonged and continuous growth.
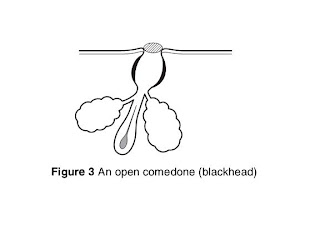
(9) Sinus tracts may appear as grouped open comedones histologically
showing a number of interconnecting keratinized
channels.(7)
Another classification is that proposed by Kadunc et al.(3)
Based on clinical appearance and relationship to surrounding
skin, acne scars are classified in this system as elevated, dystrophic,
or depressed. Other parameters include shape, consistency,
colour, and distensibility. This classification system may
also serve to assess the efficacy of various therapeutic options
based on acne scars types.(3) Kadunc’s classification is summarized
in Table 1.1.
Goodman et al. proposed a qualitative grading system that
differentiates four grades according to scar severity (Table
1.2): Grade I corresponds to macular involvement (including
erythematous, hyperpigmented, or hypopigmented scars),
whereas Grades II, III, and IV correspond to mild, moderate,
and severe atrophic and hypertrophic lesions, respectively. (10)
Interestingly, the authors consider lesion severity also according
to visibility at a social distance (> 50 cm). Moreover, since
patients may present various types of acne scars at numerous
anatomic sites (i.e., one cheek, the neck, the chest, and so
on; these single areas are defined by the authors as “cosmetic
units”), scars are further subdivided into four grades of severity
by anatomic sites involved, and the localized disease (up to
three involved areas) is classified as A (focal, 1 cosmetic unit
involvement) or B (discrete, 2–3 cosmetic units), whereas the
involvement of more cosmetic units is classified as generalized
disease, previously described in Table 1.2.
The same authors subsequently, suggested a quantitative
numeric grading system based on lesion counting (1–10,
11–20, >20), scar type (atrophic, macular, boxcar, hypertrophic,
keloidal), and severity (mild, moderate, severe). Final scoring
depends on the addition of points assigned to each respective
category and reflects disease severity, ranging from a minimum
of 0 to a maximum of 84 (Table 1.3).(11)
Finally, Dreno et al. first proposed the ECLA scale (echelle
d’evaluation clinique des lesions d’acne) (12), followed by
the ECCA grading scale (echelle d’evaluation clinique des
cicatrices d’acne) (4). According to this scoring system,
morphological aspects of lesions define the type of scars as
follows: atrophic scars (V-shaped, U-shaped and M-shaped),
superficial elastolysis, hypertrophic inflammatory scars (<2
years since onset), and keloid-hypertrophic scars (>2 years
since onset). Each scar type is associated with a quantitative
score (0, 1, 2, 3 depending on the number of lesions) multiplied
by a weighting factor that varies according to severity,
evolution, and morphological aspect. The final global score
is directly correlated with clinical severity and ranges from
0 to 540 depending on the type and number of acne scars
clinical and ultrasound correlations
Methods
Ultrasound imaging is a noninvasive technique that uses
various acoustic properties of biologic tissues. Typically, echo
signals are represented in one-dimensional diagrams (A-mode)
or two-dimensional images (B-mode).
Ultrasound of the skin is best performed by equipment
using frequencies of > 20 MHz. Using B-mode imaging,
normal skin typically shows an epidermal entrance echo, the dermal layer, and the subcutaneous layer. This technique offers
a wide range of possibilities in clinical and experimental dermatology.
It is used for the evaluation of skin tumour thickness
(e.g., basal-cell carcinoma, melanoma). Areas of research
may include scleroderma, psoriasis, and aged and photoaged
skin. Moreover, it provides an objective measurement of skin
thickness and has been utilized to assess thickness of hypertrophic
scars before and after treatment.(13)
A preliminary study was preformed in a series of
patients (N = 20) affected by various types of acne scars
in order to determine whether a correlation exists between
clinical appearance of selected scar parameters (thickness,
width, depth) with ultrasound examination. Cross-sectional
B-mode scans were obtained using a 22-MHz ultrasound
system (EasyScan Echo®, Business Enterprise, Trapani, Italy)
that allowed examination of skin sections of 12 mm in width
and 8 mm in depth.
Results
Atrophic scar•• s appear as invaginations of the skin in
which all skin layers are normally represented:
a) Icepick scars (n = 5) uniformly have a sharp, demarcated
V-shaped appearance and are characterized by a
narrow diameter at the surface (usually < 2 mm) and
a vertical extension that reaches a depth corresponding
to the deep dermis (Figure 1.1a–1.1b).
b) Boxcar scars (n = 5) uniformly present with a sharp
demarcated U-shaped appearance and are characterized
by a superficial diameter usually ranging from 2 to 4 mm
and a vertical extension that reaches a depth corresponding
to the superficial or deep dermis (Figure 1.2a–1.2b).
c) Rolling scars (n = 5) uniformly appear as large (up to 5
mm) poorly demarcated depressions of the skin; these
scars are very superficial, sometimes hardly visible, with
a vertical extension that is limited to a depth corresponding
to the epidermal thickness (Figure 1.3a–1.3b).
•• Hypertrophic and keloidal scars (n = 5) uniformly
appear as dome-shaped, localized increase of skin thickness
(Figure 4a–4b; 5a–5b); the dermis usually is less
echogenic than normal skin; in most cases, with the 22
MHz probe, keloidal scars may not be entirely visualized
because of their large size.